A protein in the lungs could be activated to treat those who suffer from allergic asthma, according to a new study.
American researchers found a protein called Piezo1 prevents a type of immune cell in the lung from becoming hyperactivated by allergens. Activating this protein using a drug called Yoda1 could be used to treat those with allergic asthma and reduce the debilitating symptoms of the condition.
Initial experiments with mice found the drug alleviated symptoms in allergen-exposed mice, suggesting it may be useful as a therapeutic tool for humans. Type 2 innate lymphoid cells - also known as ILC2s - are a type of immune cell located in the lungs, skin, and other tissues of the body.
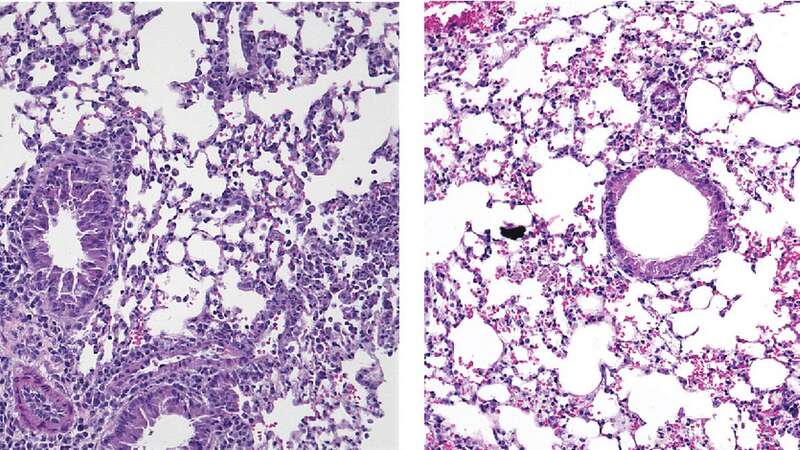
ILC2s in the lungs become activated in the presence of allergens and produce proinflammatory signals that drive the recruitment of other immune cells into the lungs. Unchecked, this can result in excessive inflammation and a tightening of the airways - making it difficult for asthma patients to breathe properly.
The study, published in the Journal of Experimental Medicine by researchers from the University of Southern California (USC), discovered that when activated by an allergen, ILC2s produce a protein called Piezo1 that can limit their activity. Professor Omid Akbari, of USC's Keck School of Medicine, said: "Given the importance of ILC2s in allergic asthma, there is an urgent need to develop novel mechanism-based approaches to target these critical drivers of inflammation in the lungs."
 Iceland issues 'do not eat' warning for Mars and Snickers treats in label mix-up
Iceland issues 'do not eat' warning for Mars and Snickers treats in label mix-up
Piezo1 forms channels in the outer membranes of cells that open in response to mechanical changes in the cell's environment, allowing calcium to enter the cell and change its activity. Dr Akbari's team found that, in the absence of Piezo1, mouse ILC2s became more active than normal in response to allergenic signals, with the animals developing increased airway inflammation. However, when treated with a drug called Yoda1 that switches on Piezo1 channels, the activity of ILC2s was reduced, airway inflammation decreased and the symptoms of allergen-exposed mice were alleviated.
The researchers' observations suggest a significant role for Piezo1 channels in ILC2 metabolism, as treatment with Yoda1 reduced ILC2 mitochondrial function and rewired the cells' energy source. Dr Akbari's team determined that human ILC2s also produce Piezo1 and tested the effects of Yoda1 on mice whose ILC2s had been replaced with human immune cells.
"Remarkably, treatment of these humanised mice with Yoda1 reduced airway hyperreactivity and lung inflammation, suggesting that Yoda1 may be used as a therapeutic tool to modulate ILC2 function and alleviate the symptoms associated with ILC2-dependent airway inflammation in humans," Dr Akbari said.
"Future studies are therefore warranted to delineate the role of Piezo1 channels in human patients with asthma and develop Piezo1-driven therapeutics for the treatment of allergic asthma pathogenesis."
Read more similar news:
Comments:
comments powered by Disqus
































